Special Health Care Needs
Knowledge and Utilization of Sensory-Based Modifications in Pediatric Dentistry
129 - Familiarity, Utilization, and Perceived Effectiveness of Sensory-Based Strategies in Pediatric Dental Care

Jamie Chang, DDS
Pediatric Dental Resident
Herman Ostrow School of Dentistry
Herman Ostrow School of Dentistry of USC
Hacienda Heights, California, United States- LS
Lily Shkhyan, MS, BS
USC Chan Division of Occupational Science and Occupational Therapy
- SR
Shannon Roux, BA, MAT
USC Chan Division of Occupational Science and Occupational Therapy
- JP
Jose Polido, DDS, MS
Herman Ostrow School of Dentistry of USC and Children’s Hospital Los Angeles
- LS
Leah I. Stein Duker, PhD, OTR/L
Assistant Professor
University of Southern California
Los Angeles, California, United States - LS
Leah I. Stein Duker, PhD, OTR/L
Assistant Professor
University of Southern California
Los Angeles, California, United States - AA
Alexander Alcaraz, DMD
Program Director
Herman Ostrow School of Dentistry
Los Angeles, California, United States
Presenting Author(s)
Co-Author(s)
Research Mentor(s)
Program Director(s)
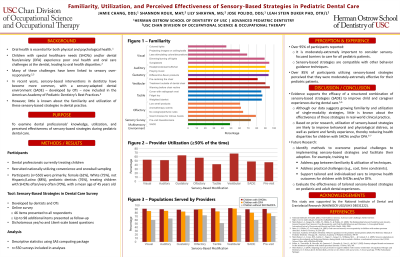
Background/Purpose: Children with special health care needs (CSHCNs) commonly experience challenges during dental care that have been linked to sensory over-responsivity, but little is known about the use of sensory-based modifications (SBMs) during dental care. Therefore, this study aimed to examine the familiarity, utilization, and perceived effectiveness of SBMs during pediatric care. Methods: A national online survey (n=46 items presented to all respondents, up to 98 additional items presented based on preceding answers) was sent to dental professionals treating children, utilizing convenience and snowball sampling. Data were analyzed descriptively using SAS. Results: Five hundred fifty dental professionals [Age-Mean(SD)=45.2(14.0); Female=62%; White=75%; Pediatric dentists=76%; In private practice=62%; Years practicing-Mean(SD)=16.6(13.2); Treating CSHCNs often/very often=70%] were included in analyses. Over 66% of respondents were familiar with SBMs across all modalities (i.e., visual, auditory, gustatory, olfactory, tactile, vestibular), with ≥63% reporting the use of at least one strategy when treating CSHCNs. Fewer participants reported knowledge (40%) or utilization (25%) of a sensory-adapted dental environment intervention. Most respondents stated that SBMs were moderately-extremely helpful ( >85%) and compatible with other basic behavior guidance techniques ( >98%). Almost 99% of participants agreed it was moderately-extremely important to consider sensory-focused barriers to care for CSHCNs. Conclusion: Most dental providers treating children are familiar with, utilize, and perceive that SBMs are effective when utilized during care. Many SBMs are simple, low-cost, and easily implemented in healthcare settings. Occupational therapists are experts in identifying and integrating SBMs and may be a valuable addition to the interdisciplinary oral care team. Research supported by the National Institute of Dental and Craniofacial Research (UG3/UH3 DE031222). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Identify Supporting Agency and Grant Number:

.jpg)