Special Health Care Needs
65 - Sensory-Adapted Dental Environment for Pediatric Patients with Sensory Processing Disorders

Nida-e-Haque Mahmud, DDS, BDS (she/her/hers)
Pediatric Dentistry Resident
UT Health San Antonio School of Dentistry
UCLA School of Dentistry, UT Health San Antonio School of Dentistry
San Antonio, Texas, United States- NK
Noorpreet Kaur, BDS, MPH
Assistant Professor/Clinical, Department of Comprehensive Dentistry, Faculty, Special Care Dentistry
UT Health San Antonio School of Dentistry, San Antonio Texas
San Antonio, Texas, United States - ML
Mei-Ling Lin, PhD, OTR
Assistant Professor
UT Health San Antonio
The University of Texas Health Science Center at San Antonio - CW
Chinyu Wu, PhD, OTR (she/her/hers)
Associate Professor
University of Texas Health Science Center at San Antonio
University of Texas Health Science Center at San Antonio - JG
Jonathan Gelfond, M.D., Ph.D.
UT Health San Antonio
- TC
Teemar Carey, DMD, MSEd
Clinical Associate Professor
UT Health San Antonio - SC
Suman Challa, BDS, MS
UT Health San Antonio
- MC
Maria-Jose Cervantes Mendez, DDS, MS
Program Director
UT Health San Antonio
San Antonio, Texas, United States - NK
Noorpreet Kaur, BDS, MPH
Assistant Professor/Clinical, Department of Comprehensive Dentistry, Faculty, Special Care Dentistry
UT Health San Antonio School of Dentistry, San Antonio Texas
San Antonio, Texas, United States - SD
Stanislaus Dyda, DDS
Interim Program Director Pediatric Dentistry
UT Health San Antonio School of Dentistry, San Antonio, TX
San Antonio, Texas, United States
Presenting Author(s)
Co-Author(s)
Research Mentor(s)
Program Director(s)
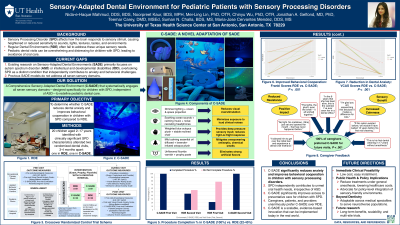
Purpose: This 8-month randomized crossover trial evaluated the efficacy of a Comprehensive Sensory-Adapted Dental Environment (C-SADE) for children with Sensory Processing Disorders (SPD) in improving behavior and reducing anxiety during periodic oral exams compared to a Regular Dental Environment (RDE). Unlike prior autism-focused research, this trial aimed to establish SPD as an independent barrier to pediatric dental care.
Methods: Children aged 2–17 years with clinically significant SPD characteristics were recruited. Caregiver-rated or self-rated Sensory Profile scores were validated by certified occupational therapists. Participants received two randomized cleanings, one in C-SADE and one in RDE, 3-4 months apart. C-SADE incorporated seven sensory adaptations: visual, auditory, tactile, gustatory, olfactory, vestibular, and proprioceptive. Outcomes included behavior (Frankl, Ohio scales), anxiety (Visual Clinical Anxiety Scale [VCAS], child-reported Visual Facial Anxiety Scale [VFAS]), physiological measures (HR, SpO2, BP), and caregiver feedback (Likert-type surveys, thematic analysis of interviews).
Results: Twenty children [Age-Mean(SD)=9.1(3.8); Male=50%; SPD=100%; Autism=20%] were enrolled. C-SADE improved behavior (Frankl: +1.65, 95% CI [1.30, 2.00], P < .001; Ohio: −1.55, 95% CI [−2.02, −1.08], P < .001) and reduced anxiety (VCAS: −2.00, 95% CI [−2.37, −1.63], P < .001; BP decrease, P= .07). Most children reported "no worries" (VFAS) in C-SADE (P < .001). Caregiver-reported anxiety decreased in C-SADE (P < .001), consistent with qualitative themes of reduced resistance and greater calmness. Post-C-SADE caregiver satisfaction increased (P < .001); all caregivers preferred C-SADE for future visits.
Conclusions: C-SADE significantly improved behavior and reduced anxiety for children with SPD, underscoring the critical need to address sensory challenges that exist beyond autism and implement tailored adaptations to ensure equitable, patient-centered pediatric dentistry.
Identify Supporting Agency and Grant Number:
Research supported by HRSA-Bureau of Health Workforce, HRSA-22-045.

.jpg)