Trauma
61 - Impact of Dental Trauma Decision-Making Pathway in Emergency Medicine

Erik P. Skoe, DDS (he/him/his)
Pediatric dental resident
Children’s National Medical Center, Washington, D.C.
Children's National Hospital
Washington DC, District of Columbia, United States
Erik P. Skoe, DDS (he/him/his)
Pediatric dental resident
Children’s National Medical Center, Washington, D.C.
Children's National Hospital
Washington DC, District of Columbia, United States
Dennis M. Ren, MD (he/him/his)
Pediatric Emergency Medicine Attending
Children's National Hospital
George Washington University School of Medicine and Health Sciences- JC
Jennifer L. Cully, DMD
Chief of Dentistry
Children's National Hospital
Washington, District of Columbia, United States - JC
Jennifer L. Cully, DMD
Chief of Dentistry
Children's National Hospital
Washington, District of Columbia, United States - MC
Mudrika Chhabra, DMD
Program Director
Children's National Hospital
Washington DC, District of Columbia, United States
Presenting Author(s)
Co-Author(s)
Research Mentor(s)
Program Director(s)
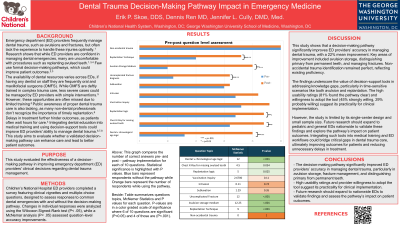
Purpose: This study evaluated the effectiveness of a decision-making pathway in improving emergency department (ED) providers' clinical decisions regarding dental trauma management.
Methods: Children’s National Hospital ED providers completed a survey featuring clinical vignettes and multiple-choice questions, designed to assess responses to common dental emergencies with and without the decision-making pathway. Changes in individual responses were analyzed using the Wilcoxon Signed-Rank test (P < .05), while a McNemar analysis (P < .05) assessed question-level accuracy improvements.
Results: Thirty-one ED providers completed the survey. A significant mean improvement in accuracy (22%) was observed post-pathway implementation (P < .001). Participants demonstrated perfect accuracy in identifying non-accidental trauma (100%) regardless of pathway use. Significant improvements were noted in key areas, including distinguishing dental from chronological age, managing uncomplicated fractures, selecting appropriate avulsion storage mediums, applying replantation logic and techniques, and addressing vaccination considerations (P < .05). Nearly half of respondents (45%) indicated a strong willingness to adopt the pathway, 29% expressing probable use. Furthermore, 81% found the pathway somewhat or extremely clear.
Conclusions: The decision-making pathway significantly improved ED providers’ accuracy in managing dental trauma, particularly in diagnosing fractures, identifying appropriate avulsion storage options, and distinguishing primary from permanent teeth. Enhanced performance in replantation decisions and significant improvements in question-specific accuracy further highlight the importance of structured decision-support tools in clinical practice. Research should continue at a nationwide level including pediatric and general EDs to codify benefits of a decision-making pathway in supporting providers’ care for dental trauma patients.
Identify Supporting Agency and Grant Number:

.jpg)