Sedation
46 - Comparison of Airmod and Capnography for Pediatric Sedation Respiratory Rates
- TK
Taj Kooner, DDS
Pediatric Dental Resident
UT Health San Antonio School of Dentistry
San Antonio, Texas, United States - CT
Courtney D. Turner, DMD
Resident
UT Health San Antonio School of Dentistry
University of Texas Health Science Center at San Antonio - CC
Claudia P. Contreras, DDS
Assistant Clinical Faculty Pediatric Dentistry/ Pre-doctoral Director
UT Health San Antonio School of Dentistry
UT Health San Antonio School of Dentistry
San Antonio, Texas, United States - SD
Stanislaus Dyda, DDS
Interim Program Director Pediatric Dentistry
UT Health San Antonio School of Dentistry, San Antonio, TX
San Antonio, Texas, United States
Presenting Author(s)
Co-Author(s)
Research Mentor(s)
Program Director(s)
Purpose: This study aimed to evaluate the accuracy of the Airmod device compared to capnography (Cap), the gold standard, in measuring respiratory rates (RR) in pediatric patients undergoing oral conscious sedation during dental procedures.
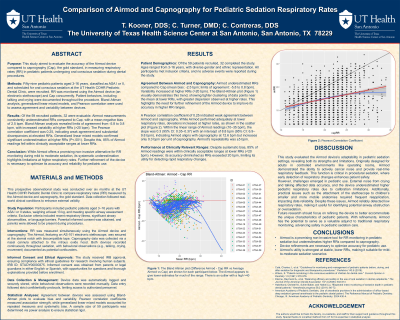
Methods: Fifty-nine pediatric patients aged 3-16 years, classified as ASA I or II, and scheduled for oral conscious sedation at the UT Health COHR Pediatric Dental Clinic, were recruited. RR was monitored using the Airmod device (an electronic stethoscope) and Cap concurrently. Patient behaviors, including talking and crying were documented throughout the procedure. Bland-Altman analysis, generalized linear mixed models, and Pearson correlation were used to assess agreement and variability between devices.
Results: Of the 59 recruited patients, 32 were evaluable. Airmod measurements consistently underestimated RRs compared to Cap, with a mean negative bias of 2.5 bpm. Bland-Altman analysis revealed limits of agreement from -5.8 to 0.8 bpm, with increased variability at higher RRs ( >20 bpm). The Pearson correlation coefficient was 0.25, indicating weak agreement and substantial discrepancies at elevated RRs. Generalized linear mixed models confirmed significant underestimation at higher RRs (P < .001). Despite this, 85% of Airmod readings fell within clinically acceptable ranges at lower RRs.
Conclusion: While Airmod offers a promising non-invasive alternative for RR monitoring during mild to moderate sedation, its systematic underestimation highlights limitations at higher respiratory rates. Further refinement of the device is necessary to optimize its accuracy and reliability for pediatric use.
Identify Supporting Agency and Grant Number:

.jpg)